Relative Clinical Efficiency and Phase 2 Biomarker Studies
Last year. Nature Reviews Drug Discovery asked the FDA’s Tatiana Prowell (Hematology & Oncology Products Division) about the most common pitfalls confronting clinical trials in oncology. She cited the late stage evaluations of biomarkers as one of three critical issues leading to regulatory failure [1]. The primary lesson: those who want to test biomarkers need to start earlier.
OncoMed’s Eric Holmgren recently expanded on the nature of the problem, at a Cytel and ASA sponsored symposium on Statistical Innovations in Clinical Development. According to Holgren, the use of biomarker testing during Phase 2 can satisfy many forward-looking objectives. The objectives to prioritize, however, should depend quite significantly on a clinical trial sponsor’s resource constraints and asset value, and in particular on pre-Phase 2 costs. He considers three scenarios to illustrate how the investment undertaken in pre-Phase 2 studies should shape the objectives of Phase 2.
Holmgren began by identifying and explaining the following account of relative clinical efficiency:
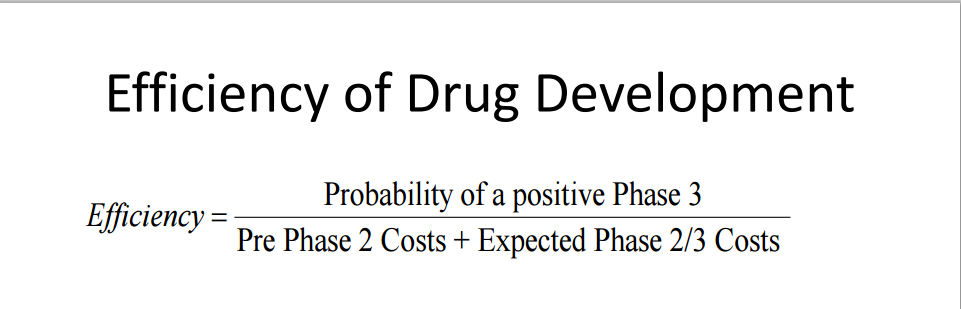
Holmgren argues that if the measurement of relative clinical efficiency is defined as it is above (as an inverse ratio between the probability of Phase 3 success and expected costs of the full spectrum of drug development), then pre-Phase 2 costs must obviously play a significant role in determining the objectives of a Phase 2 study. For example, high pre-Phase 2 costs mean that the more risk-mitigation available Phase 3 the better the reason to perform a Phase 2 study. Identifying the appropraite biomarker subpopulations can often achieve this objective [2].
Holmgren considers the following three scenarios to illustrate his analysis:
- 1: Large pre-Phase 2 Invesment
- 2: Minuscule pre-Phase 2 Investment
- 3: Small biotech with large pre-Phase 2 investment and large payoff to a successful Phase 2 study
Scenario 1: Large pre-Phase 2 Investment
This scenario involves a large pharmaceutical company, with extensive resources invested into one or more new drugs. Since pre-Phase 2 costs are already significantly high, locating subgroups with high treatment effect are necessary to increase the expected (financial) utility of a Phase 3 trial. Holmgren advises utilizing a Phase 2 biomarker trial to locate areas of treatment effect with superior promise.
Cytel Consulting adds that such Phase 3 risks can diminish even further by the careful implementation of a Phase 3 adaptive population enrichment trial [2] [3]. Such trial designs allow for different arms of a trial to study the treatment effects of a drug on different subgroups. Interim analysis typically gives sponsors the choice of continuing the trial with the population at large; or moving forward with particular subgroups that have theretofore responded quite well to the new therapy. Identifying such potential subgroups in Phase 2 indicates at least a minimal return on investment.
Scenario 2: Minuscule pre-Phase 2 Investment
Now imagine a situation where pre-Phase 2 costs are rather low. Here, relative clinical efficiency is determined entirely by the likelihood of success of a Phase 3 trial, and the expected costs of Phases 2/3.
“In this setting,” says Eric Holmgren, “the primary objective in Phase 2 should be screening for activity to see if Phase 3 should even be undertaken.”
A large pharmaceutical which performs many such Phase 2 trials is then positioned to know which therapies to bring forward to Phase 3.
Scenario 3: Small biotech with large pre-Phase 2 Investment & Large Expected Payoff
Scenario 3 involves a small biotech company which receives a large payout if (and typically only if) it can prove to a larger pharmaceutical company, that the therapy is worth the investment. Unlike in Scenario 2, the biotech only gets a payoff with a successful Phase 2 study. (By contrast, larger pharmaceuticals use Phase 2 to choose amongst several potential therapies to bring forward into Phase 3, thereby receiving a payoff based on the quality of information gleaned from Phase 2.)
As a result, biotechs should combine the risk mitigating strategies of Scenario 1 with the screening objectives of Scenario 2. However, Holmgern argues that even so, the Primary objective of a phase 2 study in this case should be to screen for activity to see if moving forward in Phase 3 is suitable. Biomarker studies can reveal the great potential of a therapeutic, and provide that extra bit of insight that might convince a potential investor of the quality of the asset.
Related Items of Interest
[1] Overcoming Prowell's Pitfalls: Cytel Weighs in on Strategies for Oncology Development
[2] 5 Reasons to Invest in Adaptive Designs for Population Enrichment
[3] Mehta Publishes Article on Adaptive Designs for Biomarker Driven Population Enrichment in Oncology
[4] Adaptive Designs for Precision Medicine: A Look at Pfizer's Xalkori Trial (Slides Attached)
[5] Speeding Early Development with Simulation & Biomarkers (Webinar Video)


